
From hospitals to community care, aged care to NDIS, data migrations aren’t just technical projects — they’re about safeguarding patient safety, protecting funding, and ensuring continuity of care. We specialise in healthcare data migrations that deliver compliance, security, and peace of mind.
Every health service faces unique challenges, but they all share one truth: bad data can compromise care and funding.
Compliance pressure: HLIS Act, and sector-specific standards (aged care accreditation, NDIS Practice Standards).
Integration complexity: Systems (WebPAS, iPM, CMI, bespoke dental/NDIS software) need to align with modern platforms.
Funding and reporting risks: Incorrect data disrupts HCP, ANZARD, NWAU, ACFI/AN-ACC, NDIS claims, or mental health reporting (e.g. HoNOS/NOCC completeness).
Operational disruption: Clinicians, carers, and administrators can’t afford downtime or broken workflows.
We bring sector-wide expertise to make migrations predictable and safe.
A proven migration framework that balances technical precision with business continuity across diverse health services:
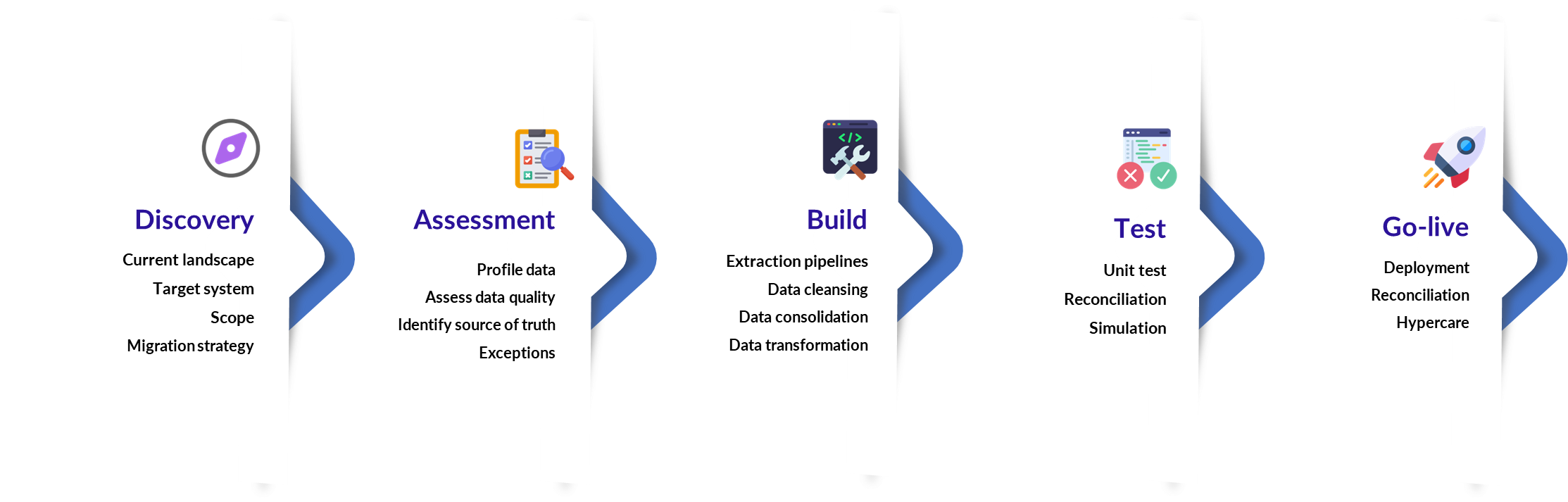
1. Assessment & Planning
2. Data Quality & Cleansing
Apply validation rules specific to your sector.
3. Secure Migration Execution
Encrypted transfers, audit logs, staged cutovers for minimal downtime.
4. Validation & Testing
Dual-run reconciliations to verify clinical, financial, and administrative data.
User acceptance testing with clinicians, carers, finance, and operations teams.
5. Optimisation & Handover
Documentation and training for IT, finance, and frontline teams.
Governance processes embedded for ongoing compliance.
Delivering a healthcare data migration isn’t just about technical execution — it’s about disciplined project management that reduces risk, keeps stakeholders engaged, and ensures outcomes are achieved on time and within budget.
Structured Methodology: We follow a phased delivery model (initiation → planning → execution → validation → closeout) aligned with PRINCE2 best practice. Each phase has clear entry/exit criteria and defined deliverables.
Governance & Oversight: A dedicated project manager oversees scope, risks, issues, and timelines, reporting through steering committees and agreed governance forums.
Agile Where It Matters: While major milestones are fixed, we use agile methods (sprints, backlog prioritisation) for data cleansing, interface testing, and reporting requirements to give flexibility and faster feedback cycles.
Executive Visibility: We provide regular progress reports and executive dashboards that translate technical progress into business impacts, so CFOs, COOs, and CIOs always have a clear line of sight.
Collaborative Engagement: Our team runs weekly project stand-ups and monthly steering committee meetings with your stakeholders to ensure alignment, transparency, and issue resolution.
Change & Risk Management: Risks and issues are logged, rated, and tracked with mitigations agreed jointly with client leads. Change requests are managed through a clear and fair process, avoiding surprises.
Knowledge Transfer: We embed client training, documentation, and handover sessions to ensure your IT, finance, and clinical teams are confident managing the solution post-migration.
Standards-first mappings using HL7 v2, FHIR AU Core and CDA, with a canonical healthcare data model to insulate downstream systems from vendor change
Deterministic patient and provider identity resolution using IHI, MRN and local keys with survivorship and audit rules
Pre-migration data quality gate with sector-specific validators
Contract tests for every interface against vendor test harnesses plus schema and vocabulary validation
Replayable integration pipelines with message versioning, idempotency, dead-letter queues and automated retries
Dual-run reconciliation during cutover, record-level variance reports and finance-grade balancing for activity and funding data
Performance and load testing with back-pressure controls and rate limits to protect source and target systems
Segmented go-live plan with blue-green or phased activation, vendor co-ordinated change windows and a documented rollback path
Full observability of interfaces, including end-to-end trace IDs, error dashboards, alerting and RPO or RTO alignment
Security controls by design, including least-privilege service identities, NASH certificate lifecycle management, encrypted transport and at-rest policies
Operability handover, including interface runbooks, support SLAs, and training for IT, clinical and finance users
Tools: Azure Data Factory, Azure Functions, SQL/ETL frameworks, Azure OpenAI for classification and categorisation of clinical notes, alerts and allergies.
Security: AES-256 encryption, zero-trust controls, ISO 27001 alignment.
Audit-ready compliance: Meet accreditation, regulatory, and audit standards.
Continuity of care: No disruption to patient, client, or resident services.
Futureproofing: Data migration as a foundation for analytics, forecasting, and AI.
Real Outcomes, Real Voices




